WHAT IS BODY DYSMORPHIC DISORDER (BDD)?
Body Dysmorphic Disorder (BDD), often called body dysmorphia, is a mental health condition where a person becomes intensely and repeatedly focused on one or more perceived flaws in their appearance. These “flaws” are usually small or invisible to other people, but to the person with BDD they can feel huge, overwhelming, and impossible to ignore.
People with BDD often:
- Spend a lot of time thinking about how they look
- Feel deeply ashamed, “ugly,” or “deformed”
- Try to check, fix, or hide the part of their body they dislike
- Find that these worries interfere with school, work, relationships, or social life
BDD is not vanity and not just “being insecure.” It’s a serious, but treatable, mental health condition. This article is for general information only and is not a diagnosis or a substitute for professional care.
IS BDD DIFFERENT FROM NORMAL INSECURITY ABOUT YOUR APPEARANCE?
Almost everyone has days where they don’t like how they look, or a feature they wish they could change. That’s totally normal.
With Body Dysmorphic Disorder, appearance worries go much further. Common differences include:
- Time: Thoughts about the “flaw” can take up hours every day
- Intensity: The distress is intense and persistent, not just an occasional bad day
- Impact: The worries get in the way of living life — school, work, social events, dating, or leaving the house
- Behaviors: The person feels driven to repeat certain rituals (like mirror checking or hiding the body part) that are hard to stop
If appearance concerns constantly dominate your day and you feel stuck in a cycle of checking, avoiding, or hiding, it may be more than normal insecurity.
BDD VS EATING DISORDERS AND SOCIAL MEDIA BODY IMAGE ISSUES
Many people ask:
- “Is body dysmorphia the same as an eating disorder?”
- “Is BDD just from social media filters and beauty standards?”
Here’s how they differ and overlap.
BDD vs Eating Disorders
- Eating disorders (like anorexia or bulimia) mainly focus on weight, shape, and food behaviors
- BDD can focus on any body part: nose, skin, hair, jawline, muscles, chest, scars, pores, and more
- Some people have both BDD and an eating disorder, but they are diagnosed and treated as related yet separate conditions
BDD vs Social-Media-Driven Insecurity
Social media can make anyone feel “not good enough” — thanks to filters, editing, and unrealistic beauty standards. That’s a real issue, but BDD often goes further:
- The distress is constant, not just after scrolling
- The person may avoid mirrors, photos, or leaving home
- They might repeatedly pursue cosmetic treatments yet still feel unhappy
Social media and cultural beauty ideals can trigger or worsen BDD, but they are not the sole cause.
COMMON SIGNS AND SYMPTOMS OF BODY DYSMORPHIC DISORDER
BDD can look slightly different from person to person, but many people share similar patterns of thoughts and behaviors.
Common thought patterns
Someone with BDD may:
- Obsess over a specific feature (or several), such as skin, nose, hairline, stomach, or muscles
- Believe that this feature makes them ugly, deformed, or “disgusting”
- Feel sure that other people notice and judge this feature
- Mentally compare their looks to others nonstop
The focus can also shift over time, for example from skin to hair, or from weight to jawline.
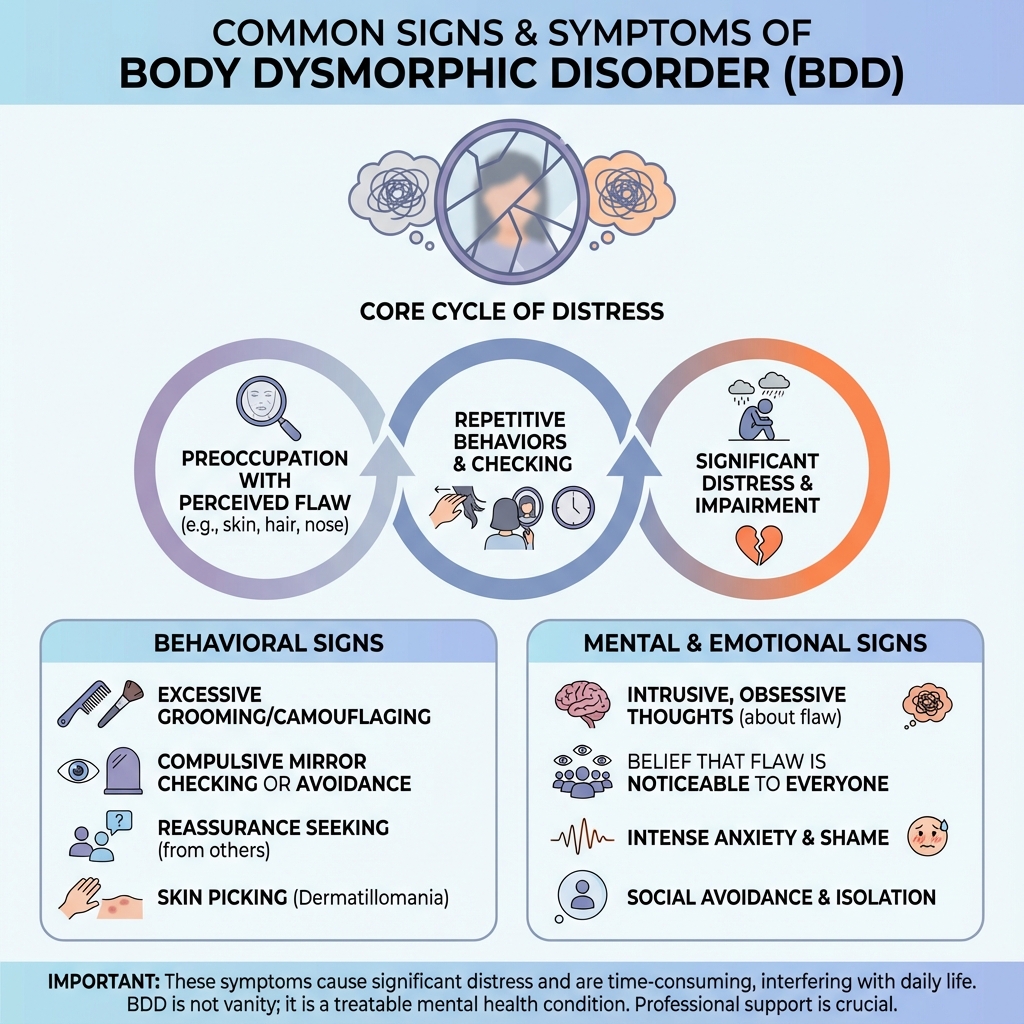
Common repetitive behaviors (rituals)
To try to cope with the distress, a person with BDD might:
- Check mirrors or reflective surfaces over and over
- Avoid mirrors completely
- Spend a long time applying makeup, grooming, or “fixing” the perceived flaw
- Pick at skin or hair to try to make it look better
- Use hats, scarves, makeup, clothing layers, or specific poses to hide the area
- Constantly ask others for reassurance (“Do I look okay?” “Is my nose weird?”)
- Compare themselves to friends, strangers, or influencers
These rituals might bring brief relief, but they usually keep the cycle going and increase anxiety in the long run.
Impact on daily life
BDD can affect:
- Social life – avoiding parties, dates, classes, cameras, or video calls
- School or work – trouble concentrating because appearance worries are so loud
- Money and time – spending a lot on products, procedures, clothing, or time-consuming routines
When body image worries start running your schedule, BDD may be at play.
HOW COMMON IS BODY DYSMORPHIC DISORDER AND WHO DOES IT AFFECT?
Body Dysmorphic Disorder is more common than most people realize. Research suggests:
- Roughly 2–3 out of every 100 people in the general population may experience BDD at some point
- Symptoms often begin in early to mid-teen years, though they can start earlier or later
- BDD can affect any gender, age group, or cultural background
It’s also especially common among people seeking cosmetic or dermatological procedures, such as skin treatments or plastic surgery, because they may feel a strong urge to “fix” the perceived flaw.
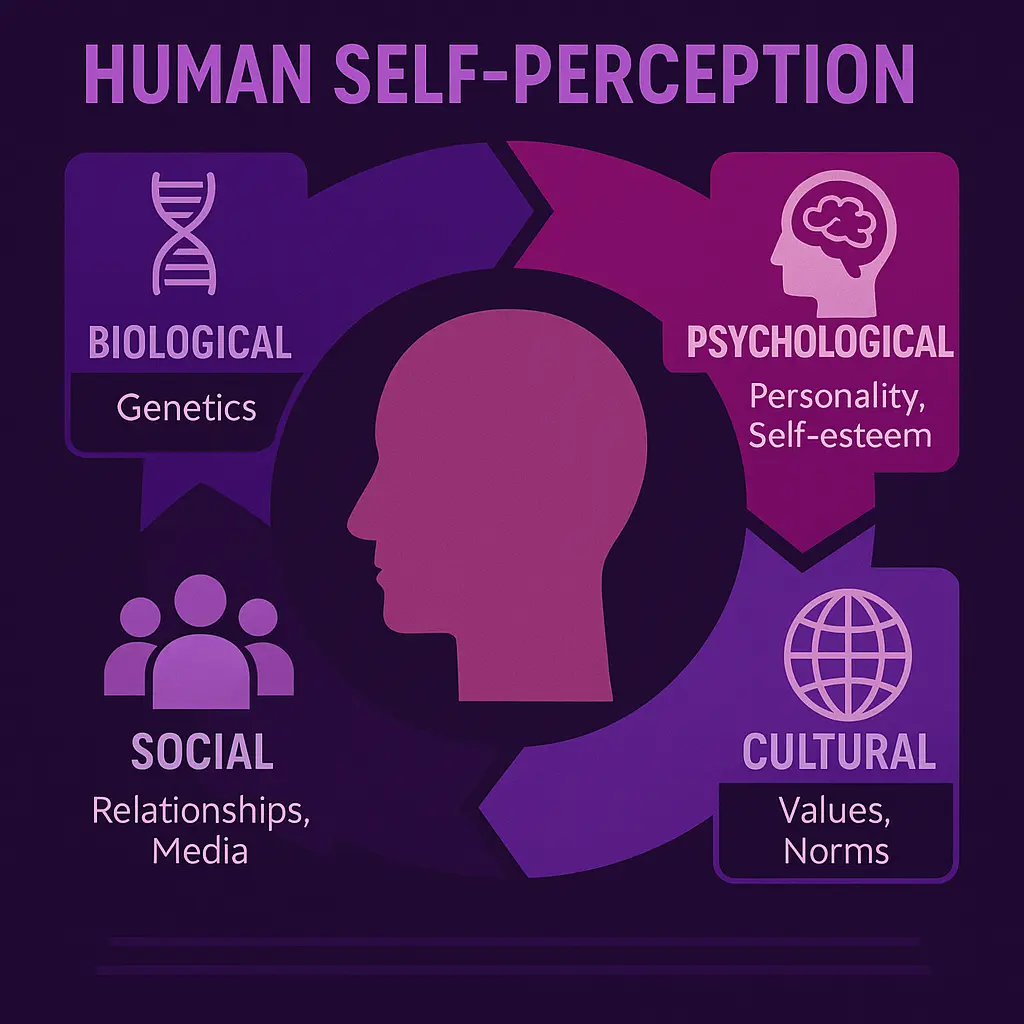
WHAT CAUSES BODY DYSMORPHIC DISORDER?
There is no single cause of BDD. It usually develops from a combination of biological, psychological, and social factors.
Biological factors
- Genetics may play a role — having family members with OCD, anxiety, depression, or BDD can increase risk
- Brain differences in areas related to perception, attention, and obsession may influence how a person with BDD processes their appearance
- Brain chemicals like serotonin (which also affect mood and anxiety) may be involved
Psychological factors
- Low self-esteem and strong self-criticism
- Perfectionism, especially around appearance or performance
- History of bullying, teasing, or criticism about looks
- A tendency to focus on details (like pores or minor asymmetries) instead of seeing the overall picture
Social and cultural factors
- Exposure to strict or unrealistic beauty standards
- Social or family environments that heavily emphasize looks
- Media, advertising, and social media filters that promote “perfect” bodies and faces
These influences can interact and pull someone into the cycle of BDD over time.
HOW DO PROFESSIONALS DIAGNOSE BDD?
Only a qualified mental health professional or medical provider can officially diagnose Body Dysmorphic Disorder. The process usually includes:
- Talking through your appearance concerns: what they focus on, how often they appear, and how they impact your life
- Asking about your behaviors: mirror checking, skin picking, excessive grooming, camouflaging, comparing, or reassurance seeking
- Exploring your emotions: shame, anxiety, sadness, or hopelessness related to how you look
- Screening for other mental health conditions, such as depression, OCD, social anxiety, or eating disorders
In general, a diagnosis of BDD requires that:
- You’re preoccupied with a perceived defect or flaw in physical appearance
- You engage in repetitive behaviors or mental acts because of that preoccupation
- These thoughts and behaviors cause significant distress or interfere with your daily life
You don’t need to “prove” that your appearance is fine. The focus is on how the thoughts and behaviors affect you.
TREATMENT OPTIONS FOR BODY DYSMORPHIC DISORDER
The encouraging news: BDD is treatable, and many people see major improvements with the right help. Treatment plans are personalized, but often include therapy, medication, or both.
Cognitive Behavioral Therapy (CBT) for BDD
CBT is one of the most effective therapies for BDD. It aims to:
- Identify and gently challenge distorted beliefs about your appearance
- Help you question the “BDD voice” that insists you look awful
- Reduce checking, hiding, and comparing behaviors through exposure and response prevention (ERP) — facing feared situations while resisting the urge to perform rituals
Over time, CBT helps your brain learn that you can handle the anxiety without relying on rituals, and that your thoughts about your appearance are not always accurate.
Medication (usually SSRIs)
Some people benefit from medication, especially if BDD symptoms are severe or occur along with depression or OCD. A healthcare provider may prescribe:
- SSRIs (Selective Serotonin Reuptake Inhibitors) or related antidepressants
These medications can reduce obsessive thoughts and the drive to perform compulsive behaviors, making it easier to engage in therapy and daily life. Medication decisions should always be made in close consultation with a doctor or psychiatrist.
Why cosmetic procedures usually don’t cure BDD
It’s very understandable to think, “If I just fix this one thing, I’ll finally feel okay.” But for people with BDD, cosmetic procedures often:
- Bring only short-term relief
- Lead to renewed dissatisfaction with the same area
- Or cause the focus to shift to a different body part
Because BDD is rooted in how you see and think about your body, not in the body itself, mental health treatment is usually much more effective than repeated cosmetic changes.
DAY-TO-DAY COPING TIPS FOR LIVING WITH BDD
Self-help strategies are not a replacement for professional care, but they can support recovery and make daily life more manageable.
Gently reduce checking and rituals
- Try to cut back on how often or how long you check mirrors, zoom in on photos, or examine your perceived flaw
- You might start by setting small limits, like “Only two mirror checks in the morning, for five minutes total”
Clean up your social media feed
- Unfollow accounts that trigger comparison or make you feel worse about your body
- Follow more diverse, body-neutral, or body-positive accounts
- Remember: most online images are filtered, posed, and carefully chosen
Separate “BDD thoughts” from facts
- When harsh thoughts appear (“You look hideous,” “Everyone is staring at you”), label them as symptoms of BDD, not objective truth
- Writing them down and then answering them with a more balanced response can be powerful
Focus on what your body can do, not just how it looks
- Notice ways your body supports you every day: walking, hugging, laughing, working, resting, learning, and connecting
- Shifting from appearance to function and experience helps loosen BDD’s grip bit by bit
Build a supportive routine
- Try to keep regular sleep, meals, and movement
- Gentle exercise, mindfulness, or grounding techniques can reduce stress and make symptoms slightly easier to handle
HOW TO SUPPORT SOMEONE WITH BODY DYSMORPHIC DISORDER
If you care about someone who may have BDD, it can be hard to know what to say or do. A few guiding principles:
- Validate their feelings, even if you don’t see the flaw
- Instead of “You’re being silly” or “You look fine,” try “I can see this really upsets you. I’m here for you.”
- Avoid endless reassurance
- Answering “Do I look okay?” a hundred times a day may unintentionally feed the cycle
- Gently pivot toward emotions and support: “I can tell this is really painful. How can I support you in getting help?”
- Encourage professional help
- Offer to help them find a therapist, book an appointment, or go with them for support
- Remind them that seeking help is a sign of strength, not weakness
- Learn about BDD together
- Understanding that it’s a recognized, treatable condition can reduce shame and increase hope
WHEN TO SEEK HELP?
BDD can be linked with high levels of distress, depression, and suicidal thoughts for some people. If you or someone you know:
- Feels like life is not worth living
- Is thinking about self-harm or suicide
- Has a plan or intent to hurt themselves
- Is in immediate danger
…this is an emergency, not something to handle alone.
Contact your local emergency services, a trusted adult, or a crisis hotline available in your country or region right away. If you can, let someone you trust know what you’re going through. Your safety matters more than anything else.
FREQUENTLY ASKED QUESTIONS ABOUT BDD
“What is body dysmorphic disorder in simple terms?”
Body Dysmorphic Disorder is a mental health condition where you feel extremely upset and preoccupied with one or more parts of your appearance, even though other people either don’t notice the issue or see it as minor.
“Do I have body dysmorphia, or am I just insecure?”
Insecurity is common. BDD is more likely when appearance worries:
- Take up a lot of your time
- Lead to repeated checking, hiding, or comparing
- Make you avoid life activities or feel unable to function normally
If that sounds like you, talking to a professional can help you understand what’s going on.
“Is BDD a type of OCD?”
BDD is in the same family as obsessive-compulsive and related disorders. Like OCD, it involves intrusive thoughts and repetitive behaviors. But in BDD, these obsessions and compulsions are specifically focused on appearance.
“Can you recover from body dysmorphic disorder?”
Yes. Many people with BDD experience major improvement — and sometimes full recovery — with treatments like CBT and, in some cases, medication. Recovery might be gradual, but change is absolutely possible.
“Can teenagers have BDD?”
Yes. BDD often starts in early or mid-teens, but it can affect people of any age. Early support can make a big difference in how severe and long-lasting symptoms become.
“Is BDD caused by social media?”
Social media doesn’t directly cause BDD, but it can intensify comparison and pressure to look “perfect.” For someone already vulnerable, that can contribute to or worsen symptoms.
FINAL THOUGHTS: YOU ARE MORE THAN A REFLECTION
When you live with Body Dysmorphic Disorder, it can feel like every mirror, camera, or reflection is an enemy — and that your worth begins and ends with how you look. But BDD is not your fault, and it does not define your value as a person.
You are more than a single feature. You are more than a photo, a filter, or an angle.
If you recognize yourself in this article, consider it a gentle nudge to reach out — to a doctor, a therapist, a trusted friend, or a mental health professional in your area. You deserve support, and you do not have to carry this alone.